Abstract
Background Multiple myeloma (MM) is a hematological malignancy with proliferation of monoclonal plasma cells which has complex genetics and prognostic heterogeneity. It involves a variety of primary genetic abnormalities, including t (4; 14), t (11; 14), t (14,16) and hyperdiploid karyotypes, as well as secondary genetic abnormalities, including chromosome copy number abnormalities (1q21+, 1p-, 13q-, 17p-, etc) and secondary translocations like MYC.
As the most common secondary genetic event, 1q21+ occurs in about 30-40% of NDMM patients while the proportion is especially higher in Chinese population, accounting for 59.7% (96/161) by a domestic study in 2022, it is closely related to the situation that MM patients may have long disease duration and late stage when initial diagnosed in China.
Despite its frequency, considerable debate remains regarding to the prognostic impact of 1q21+ in NDMM, 1q21 status hasn't been included among the high-risk markers listed by the IMWG R-ISS stage, and neither in Chinese guidelines. If 1q21+ is included as one of the poor prognostic factors, it will greatly increase the proportion of high-risk patients in NDMM patients. So, our center has begun to take 1q21 seriously as a heterogeneity problem for clinical discussion.
Methods 248 NDMM patients admitted in The First Affiliated Hospital of Soochow University from September 01, 2018 to August 31, 2021 of a VRD clinical study, with VRD in combination with ASCT or VRD treatment for 8 cycles, were retrospectively analyzed. 135 cases (54.4%) had 1q21+ by CD38-sorted fluorescence in situ hybridization (FISH), among which 153 patients were compared for the involved genes by CytoScan, focusing on the clinical characteristics, treatment response and prognostic significance by combining FISH and CytoScan technology complementary.
Results Among the 248 NDMM patients, 54.4% patients with 1q21+ were more likely to have anemia, hypoalbuminemia, renal insufficiency, high lactate dehydrogenase and high proportion of R-ISS-III stage, and are more likely to be combined with 13q14 deletion, t(4;14), and 1p deletion,and they are all at middle-risk or high-risk groups defined by Prognostic Index score.
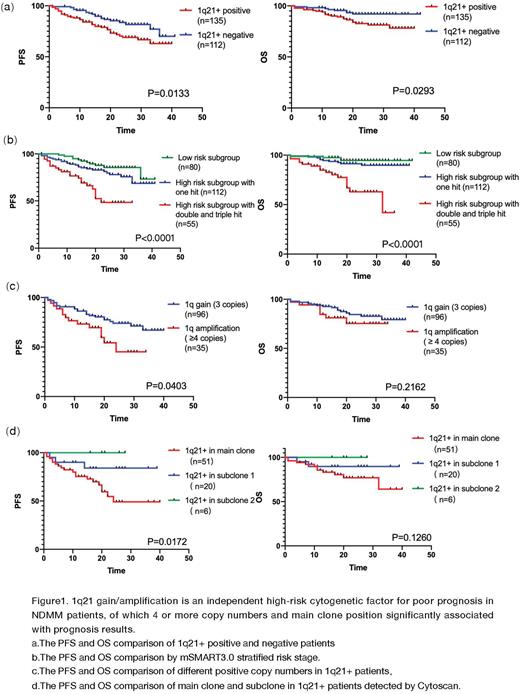
Multivariate analysis showed that 1q21 gain/amplification was an independent adverse prognostic factor (PFS HR=2.358, 95%CI 1.286-4.324, P=0.006; OS HR=2.598, 95%CI 1.050-6.425, P=0.039). 1q21+ subgroup had an inferior outcome (PFS P=0.0133, OS P=0.0293) (Figure 1a). According to the mSMART3.0 stages, double-hit and triple-hit group had the worst prognosis, with a median PFS of 22 months and a median OS of 32 months. Both PFS and OS were clinically significant (P<0.0001), as shown in Figure 1b. Furthermore 1q21 amplification with more than 4 copy numbers had a shorter PFS than 1q21 gain with 3 copy numbers (24 months vs not reached, P=0.0403), but the OS difference hasn't been not clinically significant (Figure 1c). The positive proportion of 1q21 had no effects on prognosis,while the status of 1q21 in the main clone rather than in the subclone defined by CytoScan when the proportion of abnormal clone populations are differed more than 30%, was an adverse factor affecting the prognosis (PFS P=0.0172, OS P=0.1260). (Figure 1d). ASCT plays an important role in the prognostic survival of 1q21 gain and amplification patients (P<0.05). Outcomes of 1q have been widely discussed in CRD/CTD scheme of Myeloma XI, KRd/KCD scheme of FORTE, VRD/PAD of HOVON65 and so on, our study focusing on the patients with VRD +/- ASCT is also unique, demonstrating that the prognosis of 1q21+ in VRD scheme is also poor, but ASCT can overcome the adverse effects significantly.
Conclusions Patients with 1q21+ have clinically significant end-stage organ damage and higher tumor burden, more likely to combine 13q14-, t(4;14), 1p32- and other cytogenetic abnormalities. 1q21+ is an independent high-risk cytogenetic factor for poor prognosis in NDMM patients, of which 4 or more copy numbers and main clone position significantly associated with prognosis results.
By combining FISH, CytoScan and other technologies with related abnormalities such as 1q21+,17p-, 1p32-,t (4;14), t(14;16), etc., clinical characteristics, efficacy evaluation, and prognosis can be analyzed more accurately, aiming to identify patients with poor prognosis earlier and enhancing the possibility of moving forward to the treatment strategy based on risk stratification in the future.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal